Theresa Samy, Assistant Director of Nursing, National University Hospital, Singapore
Oleh Amit Roy Choudhury
Meet the Women in GovTech 2025.
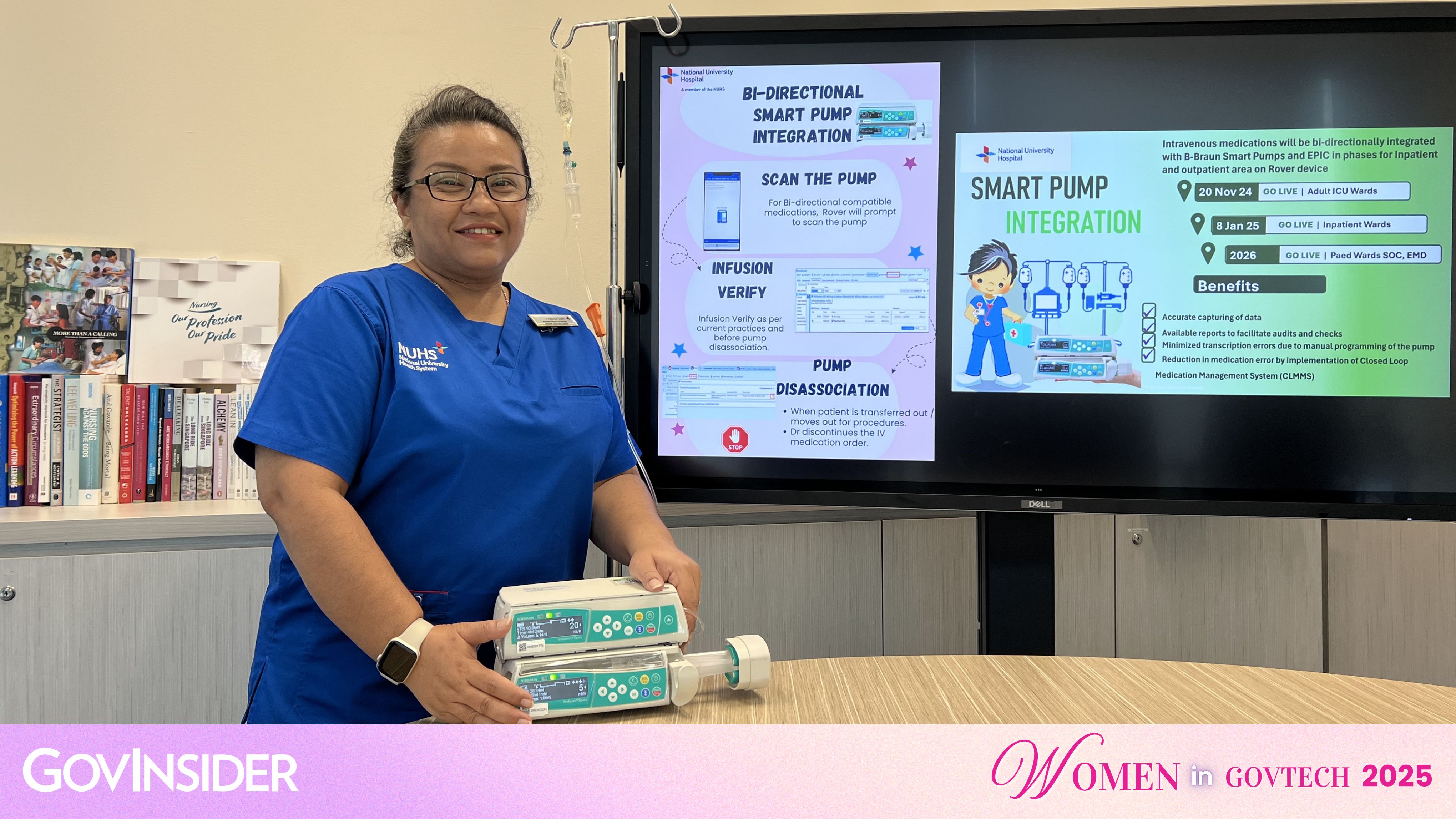
Theresa Samy, Assistant Director of Nursing, National University Hospital, shares her journey. Image: NUHS
1) How do you use your role to ensure that technology and policy are truly inclusive?
I use my role to bridge clinical practice, technology, and policy, ensuring inclusivity begins at the requirements planning stage. This involves defining needs and advocating for critical features, such as multilingual patient apps and adjustable fonts for nurses of all ages.
Policies are vital for guiding adoption, including reviews of AI tools for privacy and equity. To ensure sustainability and good adoption, flexible learning options are essential to empower all staff, not just the tech-savvy. We maintain a continuous feedback loop to refine systems, always focusing on meeting real-world needs.
My ultimate focus is advancing inclusivity by strategically harnessing technology to create seamless connections, thereby enhancing patient experiences and improving care outcomes.
2) What’s a moment in your career when you saw firsthand how technology or a new policy changed a citizen’s life for the better?
The moment was during the early days of the implementation of the National Electronic Health Record system (NEHR) and Health Hub.
These initiatives transformed care by giving clinicians a unified view of patient records and empowering citizens to manage their health.
I vividly recall an incident when I was assisting a doctor with a patient who could not articulate her chronic conditions; the National Electronic Health Record (NEHR) provided her complete history, enabling a safe and holistic treatment plan.
The Health Hub further allowed patients to access prescriptions and appointments, fostering confidence and health literacy. This experience reinforced my belief that technology, especially when supported by a strong policy, can bridge gaps and create high-quality patient-centred care.
3) What was the most impactful project you worked on this year, and how did you measure its success in building trust and serving the needs of the public?
It was a project that combined clinical workflow optimisation with patient-centred care.
Its goal was to balance safe, high-quality care for patients while reducing workload stress for nurses.
We streamlined documentation, improved resource allocation using technology, and introduced patient education tools for self-learning.
To cite an example of an initiative arising from this project, we implemented an optimisation utilising automated templates and shortcuts within the Electronic Medical Record to reduce the documentation burden, which resulted in a saving of a good 120 hours across the healthcare entities within the National University Health System cluster!
During the same period, another initiative implemented the bedside terminal to enable patients to enrol in specific education topics, allowing for self-directed learning at their own pace.
Success was measured through improved patient satisfaction, reduced documentation time, and positive staff and patient feedback.
This initiative-built trust developed through empowering patients and supporting nurses, proved that thoughtful planning and collaboration can create sustainable improvements in care delivery and strengthen confidence in our healthcare system.
4) What was one unexpected lesson you learned this year about designing for real people? This can be about a specific project or a broader lesson about your work.
This year, I learnt that simplicity often outweighs sophistication.
While designing digital tools, we focused on advanced features, but feedback revealed that ease of use mattered most in fast-paced clinical settings. They needed intuitive systems that fit seamlessly into workflows.
We then shifted to prioritise fewer clicks, clearer navigation, and more accessibility features like adjustable fonts. This experience reinforced our understanding that empathy must guide design - active listening and observing real-world use ensures technology supports care rather than complicates it.
5) We hear a lot about AI. What's a practical example of how AI can be used to make government services more inclusive and trustworthy?
Artificial intelligence (AI) has impressed us with its ability to foster inclusiveness by enabling predictive and personalised services.
An example of this is a fall risk predictor tool developed in-house, which was built to complement the nurses’ efforts in identifying patients with high fall risks in a timely fashion, allowing for prompt interventions.
Similarly, ambient speech-to-text tools help improve documentation time with precise transcription. When implemented with responsible governance, AI becomes a tool for equity, improving safety and access for diverse populations.
6) How are you preparing for the next wave of change in the public sector? What new skill, approach, or technology are you most excited to explore in the coming year?
As healthcare is moving towards being digital by default, AI is one of its primary facilitators.
I am excited about the magnitude of opportunities that lie ahead.
Improving literacy in the areas of data analytics, as well as the capabilities to leverage AI, will not just improve productivity but also enhance our ability to predict ahead.
The ability to interpret and apply data in an ethical manner is constantly evolving to ensure that security and patients’ best interests are maintained as a priority. This preparation for our workforce is crucial for resource maximisation and optimising patient care.
I am excited to further focus on building adaptability and resilience among teams to embrace innovations and process redesigns in confidence. The future demands not just technical skills but the ability to lead inclusively, ensuring advancements serve all citizens equitably.
7) What advice do you have for public sector innovators who want to build a career focused on serving all citizens?
To lead with empathy!
The second is to always remain curious because that is where opportunities will arise. Whilst technology and policy are powerful, the success of these implementations is dependent on the ability to address the gaps and pain points in a streamlined and optimised manner.
The good adoption rate of an initiative is also a critical indicator of success.
It is also important to plan for the early engagement of essential stakeholders and to embrace continuous learning, as innovation is not static, and being adaptable is key.
We must also remember to build strong collaborations across disciplines because inclusivity requires diverse perspectives.
Most importantly, we must measure success beyond quantitative metrics - look instead for trust, confidence, and improvements in experiences among those you serve.
A career in public service is about the impact and the meaningfulness of what is delivered, and that will start when we prioritise people at the centre of decisions and in healthcare, where our patients are our focus, regardless of care settings.
8) Who inspires you to build a more inclusive and trustworthy public sector?
I am inspired by my fellow nurses from different care settings who navigate complex systems daily.
Their resilience and feedback have shown me, in ways more than one, why inclusivity is essential.
Nurses inspire me through their commitment to care despite every challenge faced.
To subscribe to the GovInsider bulletin, click here.
They serve with a desire for a better outcome for the patients under their care; they are collaborators in initiatives that support making work processes better and are avid supporters of fellow colleagues implementing new initiatives.
Patients inspire me when they provide feedback on initiatives and are honest in their suggestions for improvement in one way or another.
The leaders who champion innovations with ethics and empathy inspire me and give the work we do meaning. These inspirations drive my passion to ensure that every policy and tool we implement reflects equity and trust.
9) If you had an unlimited budget, what would your dream project be?
My dream project is an integrated healthcare ecosystem that ensures patients receive timely care with just a call. A centralised, district-based hotline would route requests to the appropriate provider for immediate consultation.
Complementing this, an AI-driven home monitoring system would track patient conditions, trigger alerts, and support treatment compliance.
The platform would seamlessly connect primary, acute, outpatient, and community care, accessible via mobile devices, offering multilingual education, predictive alerts, and real-time telehealth.
For clinicians, intelligent workload balance and automated documentation would optimise efficiency. Crucially, this inclusive system would prioritise accessibility for all, regardless of digital literacy or socioeconomic status.
10) Outside tech, what excites you the most?
Whilst clinical nursing remains the cornerstone of acute care, inspiring the younger generation of nurses to embrace informatics creates new opportunities to transform patient outcomes.
Mentoring and coaching them to build confidence and capability adds another level of meaningfulness to the work I do; it is nothing short of a privilege to be part of their journey - watching them thrive and grow into leaders who share the vision for excellence.
Collaborating with like-minded teams and fostering a culture of learning energises me because it strengthens both patient care and the future of nursing.